The UK has a proud legacy in spinal cord injury (SCI) care. It was here, at Stoke Mandeville Hospital, that professor Sir Ludwig Guttmann pioneered a model of rehabilitation that placed the patient at the centre of care – a legacy that helped launch the Paralympic movement and shaped global standards. But today, that legacy is under threat.
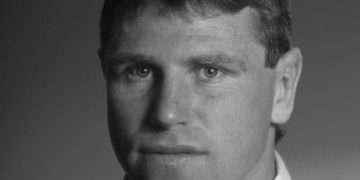
As chair of the all-party parliamentary group (APPG) on Spinal Cord Injury, I’ve heard from clinicians, researchers, charities, and – most importantly – people living with SCI. Their message is clear: the system is failing them. What should be a pathway of recovery has become a maze of delay, fragmentation, and inequality.
This is not just a healthcare issue. It is a question of dignity, equality, and national leadership.
Every two hours, someone in the UK sustains a spinal cord injury. Whether through trauma or illness, they are thrust into a system that lacks the infrastructure to support them. Over 105,000 people are living with SCI; that’s 4,700 new injuries annually. With a rapidly ageing population and more non-traumatic causes, demand is increasing while capacity has flatlined. Rehabilitation beds are scarce. Discharge planning is inconsistent. Housing is often inaccessible. Psychological support is patchy at best. And there is still no national registry to track outcomes or measure progress.
One Spinal Injuries Association member put it starkly: “Specialist spinal services are required for rehabilitation and are a non-negotiable part of recovery. We are talking about managing a condition that requires lifelong support from a health service, which if it fails can have devastating consequences.”
Our inquiry found that even basic needs are routinely unmet. Danny Byrne, for example, was left on a hard trolley in A&E for over eleven hours and developed a Grade 4 pressure ulcer. He spent five months on bedrest due to unsuitable care. Another patient, Dave Eastham, described his rehabilitation as “like being reborn again, unable to do the simplest of tasks.” These are not tragic anomalies; they are symptoms of systemic neglect.
The APPG’s report calls for a national spinal cord injury strategy – a framework to replace the current patchwork with coordinated, person-centred care. Our recommendations span five key areas: rehabilitation, workforce, community care, data, and research. The strategy is phased:
- Immediate priorities (1–2 years): stabilise the system and address urgent gaps.
- Medium term (3–5 years): build resilience through workforce development and community integration.
- Long term (5–10 years): embed a joined-up SCI strategy within the NHS 10-year plan.
This is not just about improving outcomes for SCI patients. It is about setting a precedent for how we treat long-term neurological and complex conditions – stroke, brain injury, MS, MND – all of which suffer from similar fragmentation.
We must also confront the absence of national oversight. Without data, we cannot plan. Without standards, we cannot hold systems accountable. Without leadership, we cannot drive change.
Tim Clare, a spinal cord injured patient, described his experience in a general hospital: “Virtually every aspect of my health deteriorated except for the cyst for which I was admitted. This was particularly distressing as the methods of avoiding or treating these other problems have been well established by specialist medical practice and have been part of my daily life for many years.”
These failures are not just clinical – they are political. They reflect a lack of strategic vision and a reluctance to invest in long-term, preventative care. Yet the moral and economic case for reform is overwhelming: coordinated SCI care reduces hospital readmissions, lowers lifetime public sector costs, and allows people to live independent, productive lives.
This report is not an end – it is a beginning. A blueprint for reform. A challenge to government to act.
We now need ministers to respond and commit to a National Spinal Cord Injury Strategy that restores the UK’s place as a global leader in rehabilitation, research, and inclusion. Anything less is a betrayal of the values we claim to uphold.
Let us move from platitudes to policy, from crisis management to coordinated care. Let us honour our legacy not with words, but with action, and build a system worthy of the people it serves.
Politics.co.uk is the UK’s leading digital-only political website. Subscribe to our daily newsletter for all the latest news and analysis.
The post Andy McDonald MP: ‘The system is failing spinal cord injury patients – we need a national strategy now’ appeared first on Politics.co.uk.